Insulin resistance can serve as an early alert for being at risk of developing prediabetes or type 2 diabetes. What does being insulin resistant mean? What health habit changes can diminish and maybe even derail that risk? Let’s take a look.
Insulin Resistance Explained
Insulin is the vitally important hormone that helps the body use the energy in the food we eat and manage blood glucose levels.
Often, you’ll hear people describe insulin as a key that unlocks the energy in the food we eat. This is because insulin helps glucose get into the body’s cells. Once the glucose is received it can be used by the body as energy for everything from making your organs function to moving muscles and forming thoughts.
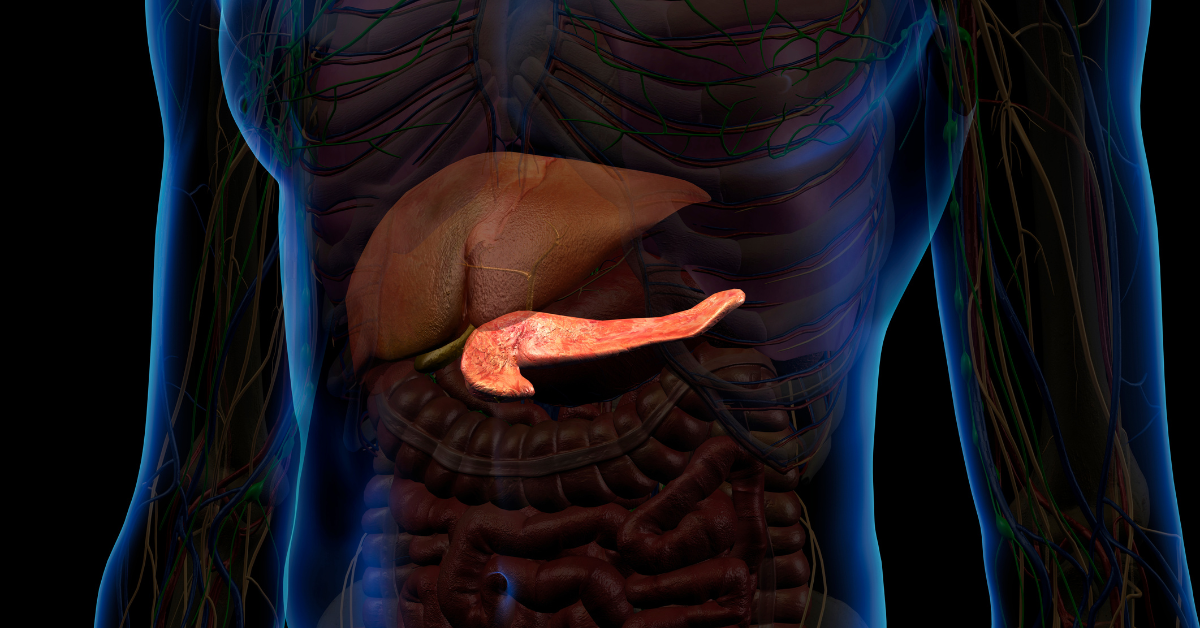
Insulin also plays an important role in how the liver processes blood glucose. Insulin signals the body to store the “extra” blood glucose (not needed by the body for immediate needs) in the liver so that it can be used later. And when that stored blood glucose is needed for energy, insulin alerts the liver to release what’s been stored.
When this all works as designed the body gets the energy it needs to function and blood glucose levels stay fairly even. However, when this process doesn’t go to plan then high levels of blood glucose remain in the bloodstream and aren’t taken in by the body’s cells or liver. As the pancreas releases more and more insulin in response to the ongoing elevated glucose levels, over time the cells can be less responsive and even stop responding all together. This is called insulin resistance.
If left alone, having chronically high blood glucose levels (known as hyperglycemia) damages the body. As blood circulates the blood vessels and nerves are damaged. Over time, every major organ: the heart, liver, kidneys, eyes, brain, etc. are affected.
As the body experiences hyperglycemia again and again over time it can lead to prediabetes and type 2 diabetes. Insulin resistance can be experienced by people with type1 diabetes as well, but it is more commonly associated with type 2 diabetes.
Addressing Insulin Resistance
Genetics, age, and health habits all influence the development of insulin resistance. While you cannot change your genetics or age, here are 6 actions you can take to counter insulin resistance.
- Move more. Physically moving and exercising your body improves insulin sensitivity. Exercise helps the muscles use the glucose in the bloodstream and insulin to regulate glucose levels.
- Eat more whole foods. Whole foods are less processed and tend to have more fiber. Because of these factors, digestion is slower (than with highly processed foods), and blood glucose levels tend not to spike (rise so dramatically) after eating.
- Get better sleep. Your body needs enough sleep for it to be restorative. This helps the body release stress and regulate various hormones. For most people this means 6 to 8 hours of sleep each night.
- Manage stress levels. When stressed the body releases hormones, most commonly cortisol and adrenaline. These hormones have a direct effect on how well the body uses the insulin released into the bloodstream.
- Stop smoking. If you smoke, quit. Smoking causes inflammation that hampers the absorption of insulin and contributes toward developing insulin resistance.
- Lose weight. Being overweight is recognized as a risk factor for developing insulin resistance. Losing as little at 5%-7% of total body weight can have a positive effect on insulin resistance.
Taking Positive Action
There are actions you can take to slow down and maybe even stop the development of insulin resistance. If you are struggling to make progress, start small and focus on one area: exercise, diet, managing stress. The most important thing is to start.

